Bilio Pancreatic Diversion
Bilio Pancreatic Diversion
Biliary Pancreatic Diversion with Duodenal Switch Surgery (BPD/DS) is a bariatric or weight loss surgery for extremely obese patients who have not been successful losing weight through dieting, exercise and medication.
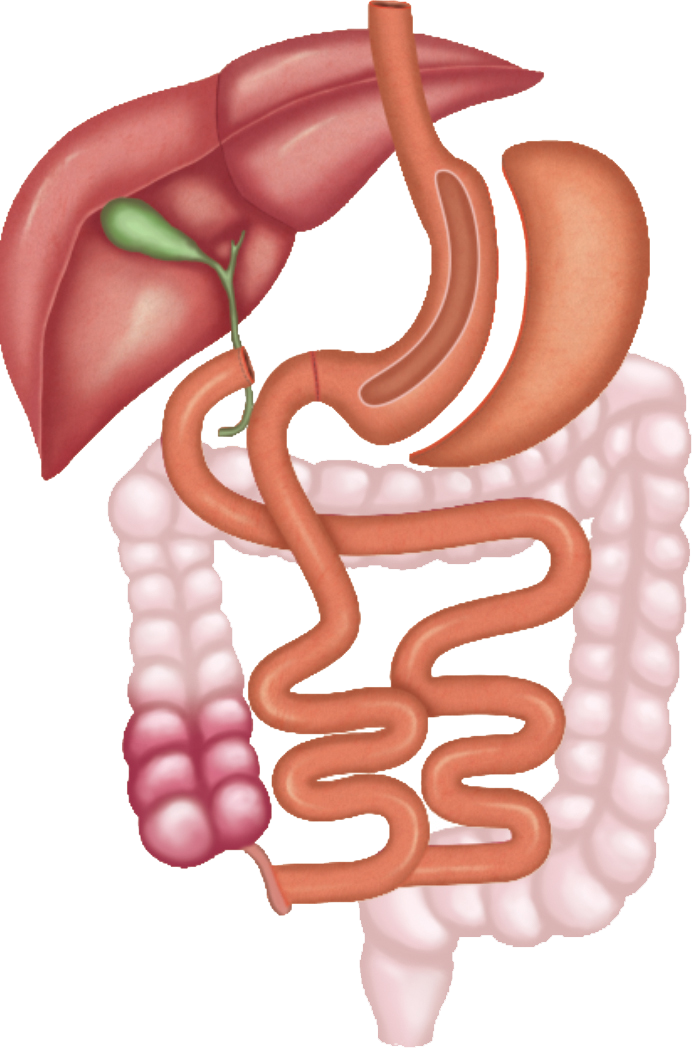
BPD/DS is a complex, 3-stage procedure that involves the following:
- Removal of a large section of the stomach, so that it holds less food
- Bypassing the upper part of the small intestine where most of the digestion takes place
- And changing the normal function of bile in the digestion process
The goal of the surgery is to make you feel full quicker so you don’t overeat, and absorb fewer calories by the modifications made in the small intestine and bile gland.
BPD/DS has been shown to help reduce obesity and related illnesses, including heart disease, high blood pressure, and especially type 2 diabetes.
Disease Overview
Obesity is a chronic condition in which there is an excessive accumulation of fat in the body. Obesity is defined as a Body Mass Index (BMI) of 30 to 34.9 and extreme or morbid obesity is defined by a BMI of 40 or more. When a person’s BMI is 50 or higher, it is referred to as super obesity. Obesity is a global problem affecting people of almost all age groups and is associated with a greatly increased risk of chronic diseases.
Indications
Bariatric surgery may be recommended for obese patients when non-surgical options such as diet, exercise and medication are unsuccessful in reducing weight.
You are a candidate for biliary pancreatic diversion with duodenal switch surgery if your body mass index (BMI) is greater than 50, or if you have a BMI greater than 40 with serious health problems.
Health conditions associated with obesity include:
- Type 2 diabetes
- Heart disease
- High blood pressure
- High cholesterol
- Sleep apnoea
- Non-alcoholic fatty liver disease
- Cancer
Surgery
The Biliary pancreatic diversion with duodenal switch surgery can be performed by open or laparoscopic techniques. In the open method, a large incision is made in your abdomen. The laparoscopic method is performed through 4 to 5 small incisions. A laparoscope, a thin fibre-optic tube with a light and camera attached to its end, is inserted through one incision. The camera allows your surgeon to clearly view the operating site on a monitor. Surgical instruments are inserted through the other incisions to perform the procedure.
BPD/DS surgery combines a sleeve gastrectomy (removal of part of the stomach) with a long intestinal bypass. In the sleeve gastrectomy part of the surgery, the outer margin of the stomach is removed, leaving a banana shaped stomach, ¼ of its original capacity, that remains connected to the duodenum. This creates the restrictive portion of the surgery.
The second part of the BPD/DS surgery involves rearranging the small intestine so food does not mix with bile and pancreatic juices until the distal end of the small intestine. This creates the malabsorption part of the surgery.
The surgeon accomplishes this by dividing the first part of the duodenum between the stomach and bile duct and closing off the divided end.
The surgeon then divides the small intestine about half way down, connecting the lower portion to the open end of the duodenum. This segment is referred to as the digestive, or roux, limb.
The remaining end of the small intestine is reconnected 75-100 cm from the large intestine creating the “common channel” which allows for bile and pancreatic juices to flow and mix with the food at the distal end of the small intestine, instead of in the duodenum, thereby limiting absorption of nutrients and calories.
Post-Operative Care
Your doctor will prescribe pain relieving medications to keep you comfortable. You will be given instructions to follow regarding wound care, diet and activity such as:
- Keep the incision area clean and dry.
- Avoid strenuous exercises and lifting heavy weights
- For the first month after the procedure, eat only small amounts of soft foods
- Sip water throughout the day to prevent dehydration.
- Follow the diet regimen given to you by the dietician.
- You will require daily vitamin and mineral supplementation for life.
The success of BPD/DS surgery is based on the patient maintaining the lost weight by following a healthy diet and regular exercise.
Advantages & Disadvantages
Advantages
BPD/DS can result in substantial weight loss in a short period of time. Most patients benefit with continued weight loss for a period of 18-24 months post-surgery.
Disadvantages
- It is not possible to fully reverse the procedure due to partial removal of the stomach.
- Lifelong follow up with a physician is required for blood tests to ensure proper health and nutrition.
Risks and complications
As with any surgery there are potential risks and complications involved. The risks associated with BPD/DS surgery include:
- Problems associated with anesthesia
- DVT (blood clot in the deep leg veins)
- Damage to the adjacent organs such as the spleen, pancreas, and bile duct
- Abdominal hernia
- Bleeding
- Infection
- Gallstone formation








 +9197 2525 2596
+9197 2525 2596